Knee Implants
These articles are for general information only and are not medical advice. Full Disclaimer. All articles compliments of the AAOS
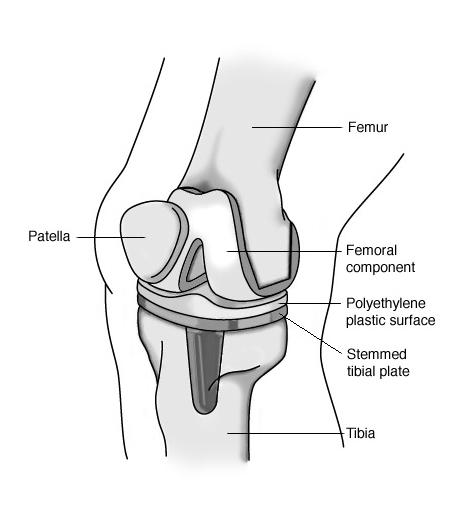
More joint replacement surgeries (arthroplasties) are performed on the knee than on any other joint. In a total knee arthroplasty (TKA), the diseased cartilage surfaces of the thighbone (femur), the shinbone (tibia) and the kneecap (patella) are replaced by prostheses made of metal alloys, high-grade plastics and polymeric materials. Most of the other structures of the knee, such as the connecting ligaments, remain intact.
Knee replacement surgery is generally recommended for patients with severe knee pain and disability caused by damage to cartilage from rheumatoid arthritis, osteoarthritis or trauma. It is highly successful in relieving pain and restoring joint function.
Implant Design
For simplicity, the knee is considered a hinge joint because of its ability to bend and straighten like a hinged door. In reality, the knee is much more complex because the surfaces actually roll and glide as the knee bends. The first implant designs used the hinge concept and literally included a connecting hinge between the components. Newer implant designs, recognizing the complexity of the joint, attempt to replicate the more complicated motions and to take advantage of the posterior cruciate ligament (PCL) and collateral ligaments for support.
Up to three bone surfaces may be replaced during a TKA: the lower ends (condyles) of the thighbone, the top surface of the shinbone and the back surface of the kneecap. Components are designed so that metal always articulates against plastic, which provides smooth movement and results in minimal wear.
- Femoral component: The metal femoral component curves around the end of the thighbone and has an interior groove so the kneecap can move up and down smoothly against the bone as the knee bends and straightens. Usually, one large piece is used to resurface the end of the bone. If only one side of the thighbone is damaged, a smaller piece may be used (unicompartmental knee replacement) to resurface just that part of the bone. Some designs (posterior stabilized designs) have an internal post with a circular-shaped device (cam) that works with a corresponding tibial component to help prevent the thighbone from sliding forward too far on the shinbone when you bend the knee.
- Tibial component: The tibial component is a flat metal platform with a polyethylene cushion. The cushion may be part of the platform (fixed) or separate (mobile) with either a flat surface (PCL-retaining) or a raised, sloping surface (PCL-substituting).
- Patellar component: The patellar component is a dome-shaped piece of polyethylene that duplicates the shape of the kneecap anchored to a flat metal plate.
There are more than 150 knee replacement designs on the market today. Several manufacturers make knee implants. The brand and design used by your doctor or hospital depends on many factors, including your needs (based on your age, weight, activity level and health), the doctor’s experience and familiarity with the device, and the cost and performance record of the implant. You may wish to discuss these issues with your doctor.
Implant Construction
The metal parts of the implant are made of titanium- or cobalt/chromium-based alloys. The plastic parts are made of ultrahigh-density polyethylene. All together, the components weigh between 15 and 20 ounces, depending on the size selected. The construction materials used must meet several criteria:
- They must be biocompatible; that is, they can function in the body without creating either a local or a systemic rejection response.
- Their mechanical properties must be able to duplicate the structures they are intended to replace; for example, they are strong enough to take weightbearing loads, flexible enough to bear stress without breaking and able to move smoothly against each other as required.
- They must be able to retain their strength and shape for a long time. The chance of a knee replacement lasting 15 to 20 years is about 95 percent.
To date, man-made joints have not solved the problem of wear. Every time bone rubs against bone, or metal rubs against plastic, the friction creates microscopic particulate debris. Just as wear in the natural joint contributed to the need for a replacement joint, wear in the prostheses may eventually require a second (revision) surgery.
Implant Insertion
During a TKA, the knee is in a bent position so that all the surfaces to be replaced can be exposed. The usual approach is lengthwise through the front of the knee, just to the inside of the kneecap, although some surgeons will approach the joint from the outer side, just above the kneecap. The incision is 6″ to 12″ long. The large quadriceps muscle and the kneecap are moved to the side to reveal the bone surfaces.
After taking several measurements to ensure that the new implant will fit properly, the surgeon begins to smooth the rough edges of the bones. Depending on the type of implant used, the surgeon may begin with either the thighbone or the shinbone.
Special jigs are used to accurately trim the damaged surfaces at the end of the thighbone. The devices shape the end of the thighbone so it configures to the inside of the prosthesis. The shinbone is cut flat across the bone and a portion of the bone’s center is drilled out. The surgeon removes just enough of the bone so that when the prosthesis is inserted, it recreates the joint line at the same level as prior to surgery. If any ligaments around the knee have contracted due to pain and deformity before the surgery, the surgeon carefully releases them so that they function as close to the normal state as possible.
The prostheses are inserted, tested and balanced. The surgeon wants to be sure that the joint line is in the right place and the kneecap is accurately aligned for proper joint movement. If it is necessary to resurface the kneecap, the surgeon will apply a shaped piece of polyethylene that maintains the original width of the kneecap.
The knee replacement may be “cemented,” “cementless” or “hybrid,” depending on the type of fixation used to hold the implant in place. Although there are certain general guidelines, each case is individual and your surgeon will evaluate your situation carefully before making any decisions. Do not hesitate to ask what type of fixation will be used in your situation and why that choice is appropriate for you.