Osteotomy and Unicompartmental Knee Arthroplasty
These articles are for general information only and are not medical advice. Full Disclaimer. All articles compliments of the AAOS
Total joint replacement (arthroplasty) is a common and very successful surgery for people with degenerative arthritis (osteoarthritis) of the knee. Two other surgeries can also restore knee function and significantly diminish osteoarthritis pain in carefully selected patients. If osteoarthritis damage to your knee meets certain qualifications, a doctor may recommend either osteotomy or unicompartmental knee arthroplasty (UKA).
Osteoarthritis Damage to the Knee
A normal knee glides smoothly because articular cartilage covers the ends of the bones that form joints. Osteoarthritis damages the cartilage, progressively wearing it away. The ends of the bones become rough like pieces of sandpaper. Damaged cartilage can cause the joint to “stick” or lock when you use it. Your knee may get painful, stiff and lose range of motion. See your doctor to diagnose osteoarthritis.
Provide your complete medical history including detailed descriptions of osteoarthritis symptoms and when they began. Have you tried nonsurgical treatments such as rest, weight loss and nonsteroidal anti-inflammatory medication for pain? Does it hurt too much to get dressed, bathe or walk up stairs? The doctor will check your knee’s range of motion, ligament stability and angular deformity. He or she will observe your knees while you stand and walk, and examine your hips, feet and ankles. Both knees will probably be X-rayed.
Your doctor’s recommendation of a surgical procedure for osteoarthritis knee repair depends in part upon how it is damaged. The knee has three joints (compartments), any or all of which can be impacted by osteoarthritis:
- The inside (medial) compartment (medial tibial plateau and medial femoral condyle) is most commonly involved, producing a bowleg (genu varum) deformity.
- The outside (lateral) compartment (lateral tibial plateau and lateral femoral condyle) is sometimes involved in women or obese people, producing a knock-knee (genu valgum) deformity.
- The kneecap (patellofemoral) compartment (patella and femoral trochlear notch) may also develop osteoarthritis.
If you have early stage arthritis confined to one part of the knee, your doctor may recommend osteotomy or UKA.
Osteotomy
Osteotomy may be appropriate if you are younger than age 60, active or overweight. There must also be uneven damage to the joint, correctable deformity and no inflammation. The surgeon reshapes the shinbone (tibia) or thighbone (femur) to improve your knee’s alignment. The healthy bone and cartilage is realigned to compensate for the damaged tissue. Knee osteotomy surgically repositions the joint, realigning the mechanical axis of the limb away from the diseased area. This lets your knee glide freely and carry weight evenly on a more normal compartment.
- Proximal tibial valgus osteotomy treats arthritis of the medial compartment, correcting a knee that angles inward (varus deformity)
- Distal femoral varus osteotomy treats arthritis of the lateral compartment, correcting a knee that angles outward (valgus deformity)
The doctor may use one of several techniques to hold the joint in place (i.e., immobilization with a cast, staples or internal plate devices).
Outcome: Osteotomy relieves pain and may delay the progression of osteoarthritis. Cosmetically, the knee may not look symmetrical after osteotomy. There’s a chance you will eventually need TKA, which can be a more technically challenging procedure after you’ve had an osteotomy. Infections and other complications are possible. Depending upon how quickly you heal, you will need to walk with crutches for 1-3 months. After that you begin rehabilitative leg strengthening and walking exercises. You may be able to resume your full activities after 3-6 months.
Unicompartmental Knee Arthroplasty
Unicompartmental knee arthroplasty (UKA) may be appropriate if you are age 60 or older, not obese and relatively sedentary. Among other specific qualifications, your knee must have:
- An intact anterior cruciate ligament (ACL)
- No significant inflammation
- No damage to the other compartments, calcification of cartilage or dislocation
Your doctor will verify that your knee meets the requirements when he or she begins the surgery. (Note: If your knee does not meet the qualifications, you may need TKA.) The surgeon removes diseased bone and puts an implant (prosthesis) in its place. The two small replacement parts are secured to the rest of your knee. You can get UKA surgery on both knees at the same time if you need it.
Outcome: UKA aleviates pain and may delay the need for TKA. You get better joint motion and function because the procedure preserves both cruciate ligaments and other healthy parts of the knee. You also keep the bone stock in the kneecap joint and the other compartment, which can be helpful if you ever need conversion to TKA in the future. Complications are rare, but the new joint could develop an infection or slip out of place after surgery. For these reasons, your doctor may want to see you for follow-up visits after surgery. You will have to do range of motion and other physical therapy exercises to rehabilitate your knee. Recovery from UKA is faster than from TKA or osteotomy.
Although UKA was a controversial procedure when it was first introduced about 30 years ago, success rates have improved thanks to precise patient selection, refined surgical techniques and improved implant design. UKA has a higher initial success rate and fewer complications compared with osteotomy. Other advantages include less blood loss during surgery and cheaper cost.
Unstable Kneecap
These articles are for general information only and are not medical advice. Full Disclaimer. All articles compliments of the AAOS.
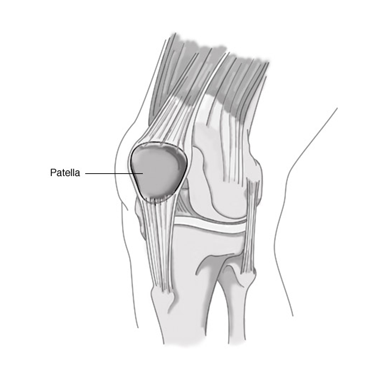
When things are “in the groove,” they’re going smoothly. That certainly is the case with your knee. As long as your kneecap (patella) stays “in the groove,” you can walk, run, sit, stand and move easily. When the kneecap slips out of the groove, problems and pain often result.
The kneecap connects all the muscles in the thigh to the shinbone (tibia). As you bend or straighten your leg, the kneecap is pulled up or down. The thighbone (femur) has a V-shaped notch (femoral groove or sulcus) at one end to accommodate the moving kneecap. In a normal knee, the kneecap fits nicely in the groove. But if the groove is uneven or too shallow, the kneecap could slide off, resulting in a partial or complete dislocation. A sharp blow to the kneecap, as in a fall, could also pop the kneecap out of place.
Symptoms
- Knee buckles and can no longer support your weight
- Kneecap slips off to the side
- Pain in the front of the knee increases with activity
- Stiffness
- Creaking or cracking sounds during movement
- Swelling
Diagnosis
During the examination, your doctor may ask you to walk around or to straighten and bend your knee. He or she may carefully feel the area around the kneecap and take measurements to determine if the bones are out of alignment or if the thigh muscles are weak. X-rays may be recommended to see how the kneecap fits in its groove. Your doctor will also want to eliminate other possible reasons for the pain, such as a tear in the cartilage or ligaments of the knee.
Treatment
If the kneecap has popped totally out of its groove (dislocated), the first step is to return it to its proper place. This process is called reduction. Sometimes this happens spontaneously; other times, your doctor will have to apply gentle force to push the kneecap back in place. A dislocation often damages the underside of the kneecap and the end of the thighbone, which can lead to additional pain and arthritis. Arthroscopic surgery can correct this condition.
If the kneecap is only partially off track (subluxated), your doctor may recommend nonoperative treatments, such as exercises and braces. Exercises will help strengthen the muscles in your thighs so that the kneecap stays aligned.
Cycling is often recommended as part of the physical therapy. A stabilizing brace may also be prescribed. The goal is for you to return to your normal activities within one to three months.
A chronic condition, in which the knee continues to be unstable, can often be corrected by surgery. For example, surgery can be used to realign and tighten tendons to keep the kneecap on track, or to release tissues that pull the kneecap off track.