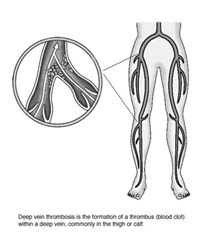
Deep Vein Thrombosis
These articles are for general information only and are not medical advice. Full Disclaimer. All articles are compliments of the AAOS
Joint replacement surgery, especially in the lower extremities, is becoming more common. Orthopedic surgeons performed about 364,000 hip replacements and about 451,000 knee replacements in 2003 (Source: National Center for Health Statistics; Centers for Disease Control and Prevention; 2003 National Hospital Discharge Survey.) The vast majority of these surgeries are very successful, and patients go on to live fuller, more active lives without pain. But no operation is without risks. One of the major risks facing patients who undergo orthopedic surgery in the lower extremities is a complication called deep vein thrombosis, a form of venous thromboembolic disease.
What is it?
Deep vein thrombosis (DVT) refers to the formation of a thrombus (blood clot) within a deep vein, commonly in the thigh or calf. This can have two serious consequences:
- If the thrombus partially or completely blocks the flow of blood through the vein, blood begins to pool and build up below the site. Chronic swelling and pain may develop. The valves in the blood vessels may be damaged, leading to venous hypertension. A person’s ability to live a full, active life may be impaired.
- If the thrombus breaks free and travels through the veins, it can reach the lungs, where it is called a pulmonary embolism (PE). A pulmonary embolism is a potentially fatal condition that can kill within hours.
Both DVT and PE may be asymptomatic and difficult to detect. Thus, physicians focus on preventing their development by using mechanical or drug therapies. Without this preventive treatment, as many as 80 percent of orthopedic surgical patients would develop DVT, and 10 percent to 20 percent would develop PE. Even with these preventative therapies, DVT and subsequent PE remain the most common cause for emergency readmission and death following joint replacement.
Contributing Factors
Although venous thromboembolic disease can develop after any major surgery, people who have orthopedic surgery on the lower extremities are especially vulnerable. Three factors contribute to the formation of clots in veins:
- Stasis, or stagnant blood flow through veins. This increases the contact time between blood and vein wall irregularities. It also prevents naturally occurring anticoagulants from mixing in the blood. Prolonged bed rest or immobility promotes stasis.
- Coagulation, which is encouraged by the presence of tissue debris, collagen, or fats in the veins. Orthopedic surgery often releases these materials into the blood system. During hip replacement surgery, reaming and preparing the bone to receive the prosthesis can also release chemical substances (antigens) that stimulate clot formation into the bloodstream.
- Damage to the vein walls, which can occur during surgery as the physician retracts, twists, folds, or manipulates veins. This can also break intercellular bridges and release substances that promote blood clotting.
Other factors that may contribute to the formation of thrombi in the veins include: age, previous history of DVT or PE, metastatic malignancy, vein disease (such as varicose veins), smoking, estrogen usage or current pregnancy, obesity and genetic factors.
After hip surgery, thrombi often form in the veins of the thigh; these clots are more likely to lead to PE. After knee surgery, most thrombi occur in the calf; although less likely to lead to PE, these clots are more difficult to detect. Fewer than one-third of patients with DVT present with the classic signs of calf discomfort, edema, distended veins, or foot pain.
Prevention
Prevention is a three-pronged approach designed to address the issues of stasis and coagulation. Usually, several therapies are used in combination. For example, a patient may be fitted with graded compression elastic stockings and an external compression device upon admittance to the hospital; movement and rehabilitation begin the first day after surgery and continue for several months; anticoagulant therapy may begin the night before surgery and continue after the patient is discharged.
- Early movement/rehabilitation: With hospital stays averaging just four to seven days after an arthroplasty on the lower extremity, early movement is imperative as well as beneficial. Physical therapy, including joint range of motion, gait training and isotonic/isometric exercises, usually begins on the first day after the operation. Pain relievers administered intravenously also facilitate early mobilization.
- Mechanical prophylaxes: Mechanical preventatives are usually used in combination with other therapies. They include:
- Lower extremity exercises such as simple leg lifts, elevating the foot of the bed, and active and passive ankle motion to increase blood flow through the femoral vein.
- Graded compression elastic stockings, which are more effective in preventing thrombi formation in the calf than in the thigh.
- Continuous passive motion, which is a logical treatment, but has not been proven effective in preventing the development of DVT.
- External pneumatic compression devices that apply pulsing pressures similar to those that occur during normal walking. They can help reduce the overall rate of DVT occurrence when used with other therapies, but they are difficult to apply and patient compliance is often a problem.
- In rare cases, a filter device may be inserted in the vein.
- Pharmacologic prophylaxis: The use of anticoagulant pharmacologic agents includes an inherent risk of increased bleeding, which must be measured against their effectiveness in preventing clot formation. The most common anticoagulants are aspirin, warfarin, and heparin.
- Aspirin is easy to administer, is low cost, has few bleeding complications, and doesn’t need to be monitored. However, it has not been proven more effective than other agents and may not be advisable for all patients. Studies have shown that aspirin has a greater protective effect for men than for women.
- Warfarin is the most commonly used agent for hip and knee replacement patients. Warfarin interferes with vitamin K metabolism in the liver to prevent formation of certain clotting factors. Because warfarin takes at least 36 hours to start working, and four to five days to reach its maximum effectiveness, it is usually started the day before surgery. Low doses are used because higher doses can cause episodes of bleeding, but the dose-response is difficult to predict and warfarin must be administered through an outpatient clinic. Warfarin can cause fetal damage.
- Heparin is a naturally occurring substance that inhibits the clotting cascade. It can come in high (standard unfractionated heparin) or low (fractionated heparin) molecular weights. Recent emphasis has been on low molecular weight heparins (LMWH) because they are more predictable and effective, with fewer bleeding complications than standard unfractionated heparin. LMWH is effective after both hip and knee joint replacement surgeries, but there is a higher incidence of bleeding when it is used after knee replacement surgery. The most commonly used and researched LMWH are enoxaparin, ardeparin, dalteparin and fraxiparine. Heparin works much faster than warfarin, so it is often administered initially and followed by warfarin therapy, or administered as a single agent.
Diagnosis
Diagnosing DVT is difficult, and current diagnostic techniques have both advantages and disadvantages. The most commonly used diagnostic tests include venography, duplex or Doppler ultrasonography, magnetic resonance imaging (MRI), and cuff-impedence plethysmography.
Venography uses a radiographic material injected into a vein on the top of the foot. The material mixes with blood and flows toward the heart. An X-ray of the leg and pelvis will then show the calf and thigh veins and reveal any blockages.
Although venography is very accurate and can detect blockages in both the thigh and the calf, it is also costly and cannot be repeated often. In addition, the injected material may actually contribute to the creation of thrombi.
Duplex ultrasonography can also be very accurate in identifying clogged veins. Projected sound waves bounce off structures in the leg and create images that reveal abnormalities. The addition of color Doppler imaging improves accuracy. This test is noninvasive and painless, requires no radiation, can be repeated regularly and can reveal other causes for symptoms. It also costs substantially less than venography. However, it is technically demanding and requires a skilled, experienced operator to obtain the most accurate results. Ultrasonography is less sensitive in detecting thrombi in the calf and it has limited ability to directly image the deep veins of the pelvis.
Magnetic resonance imaging is particularly effective in diagnosing DVT in the pelvis, and as effective as venography in diagnosing DVT in the thigh. This technique is being increasingly used because it is noninvasive and allows simultaneous visualization of both legs. However, an MRI is expensive, not always readily available, and cannot be used if the patient has certain implants, such as a pacemaker. In addition, the patient can experience claustrophobia.
Cuff-impedance plethysmography uses blood pressure checks at different places in the leg to identify possible blockages. Although once used extensively, this procedure is no longer recommended as a diagnostic tool because of its high false-positive rate.
Postoperative Treatment
The risk of developing DVT extends for at least three months after joint replacement surgery. The risk is greatest two to five days after surgery; a second peak development period occurs about 10 days after surgery, after most patients have been discharged from the hospital. Recently, the Food and Drug Administration approved the use of the LWMH dalteparin sodium in a once-daily, 14-day dosing regimen to prevent DVT after hip surgery. A common postoperative regimen is five days of heparin followed by three months of warfarin therapy. However, the length of time that therapy should continue after surgery varies depending on the agent used and individual patient considerations.
Orthopedic surgeons are continuing to research techniques, such as the use of regional anesthesia and intraoperative heparin, to reduce the risk of DVT formation. Studies have shown that using regional rather than general anesthesia can reduce the overall rate of DVT formation by up to 50 percent.
Research to identify those patients particularly at risk for DVT formation after surgery is also ongoing. Some risk factors such as weight and history have been identified. Based on these risk factors, some physicians use regular surveillance of patients, while others recommend using venography to identify those patients at risk for developing DVT. In general, orthopedic surgeons would rather avoid extended outpatient prophylaxis for all patients, preferring to focus on those most at risk.
Treatment is the same for both asymptomatic and symptomatic venous thromboembolisms. If the clot is located in the femoropopliteal vein of the thigh, treatment consists of bed rest and five days of heparin therapy followed by three months of warfarin. A clot in the calf veins does not normally require heparin treatment; outpatient warfarin treatment for six to 12 weeks is sufficient. These treatment regimens are designed to prevent the occurrence of a fatal pulmonary embolism and reduce the morbidity associated with DVT.